What does the law say about ABA coverage?
Section 10-16-104 (1.4), C.R.S
All health benefit plans issued or renewed in the state must provide coverage to assess, diagnose, and treat autism spectrum disorder (ASD).
Treatment covered includes:
- Evaluation and assessment services;
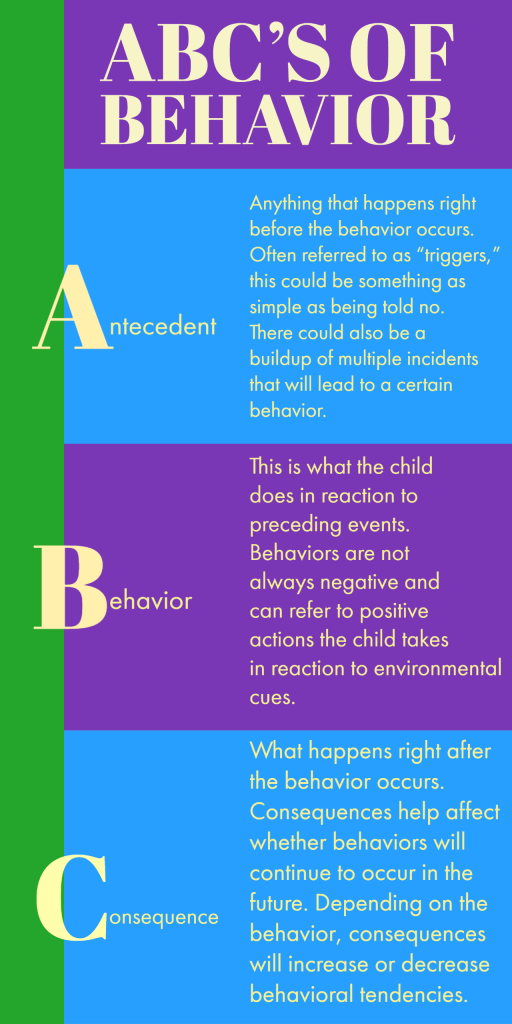
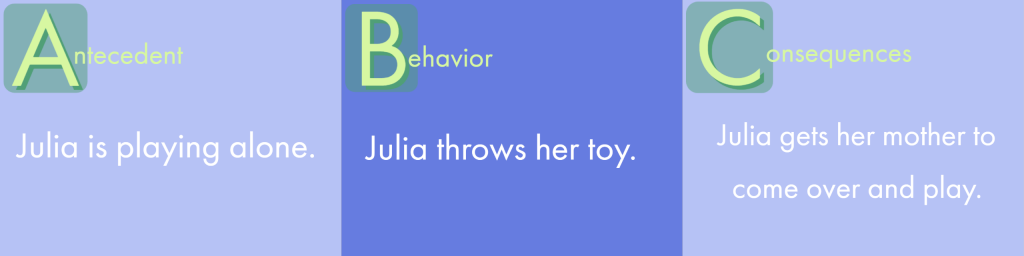
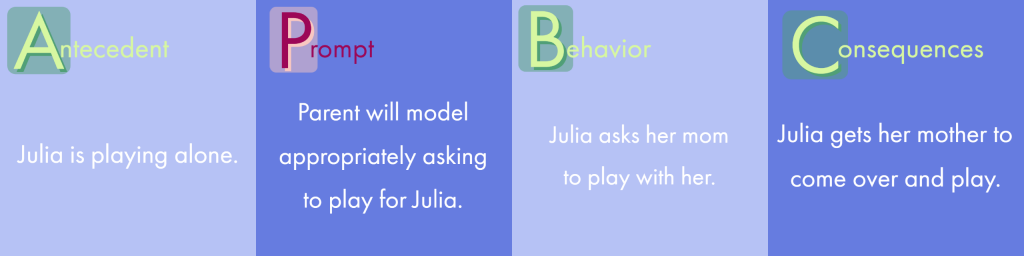
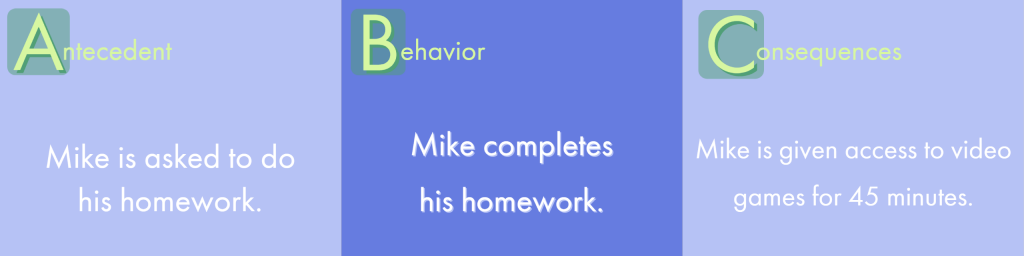
- Behavior training and management;
- Habilitative or rehabilitative care, which includes speech, occupational, and physical therapies. Speech, occupation, and physical
- Therapies may exceed 20 visits if deemed medically necessary;
- Pharmacy and medication if covered by the individual’s health plan;
- Psychiatric care;
- Psychological care, including family counseling; and
- Therapeutic care, which includes speech, occupational, and applied behavioral analytic physical therapies.
Any treatment for ASD must be deemed medically necessary. The law specifies that early intervention services, which are currently mandated under law, shall supplement, but not replace, ASD services
IMPORTANT: If your child does not have an Autism diagnosis we may be able to still help! Call us at 303-997-0305 for more information.
Although Colorado Statutes require that ABA is a covered benefit by insurance companies, many benefit plans are exempt from this statute. How does a parent know if their benefits are covered or how do they receive this benefit? Parent must know the law and understand how your individual policy in effected or not applicable to that law.
KNOWING THE LAWS
- The sate mandates only apply to policies within the Colorado Division of Insurance (DOI) jurisdiction.
- Health plans covered by the DOI include Colorado Medicaid and commercial insurance plans licensed by the state of Colorado.
- Health plans that fall outside of the DOI may include: self-funded plans, union plans, and federal employee plans.
- Mandated coverages are independent of individual policies for deductibles, co-pays, and co-insurances.
UNDERSTANDING YOUR POLICY
What type of policy do you have?
- Fully Insured: Your employer pays an insurance premium each month into a large pool with a group of other employers.
- Self-funded: Your employer pays a specific amount that is set aside for admin fees, stop-loss insurance, an an expected amount to cover doctor bills for employees.
- Union plans: Your insurance is provided by a labor union.
- Federal Employee plans: An independent group plan for federal employees that offers fee for service, HMOs and Point of Service product plans.
To find out which policy you are covered under, speak with your Human Resources Department.
VERIFY YOUR BENEFITS
If your policy falls under the Colorado DOI, then your policy MUST cover ABA! You can verify this by speaking with your HR department or calling the customer service number on the back of your insurance card.
Now that you know you are covered, what happens next?
- You need to meet the insurance requirements for ABA as medically necessary.
- Most ABA services require a pre-authorization for services.
Not to worry, we do this part for you!
If you are interested in finding out if you qualify for ABA services or just need help understanding your benefits, we can help!
We work with families every day navigating them through the insurance process to make sure their ABA is covered and you have the lowest patient responsibility possible.
We believe in high quality care and high quality service! Call us today 303-997-0305.